Advances in Prostate Screening
Prostate Cancer is Common but Can be Treated if Caught Early
Ask your Doctor about all Options for Screening and Treatment
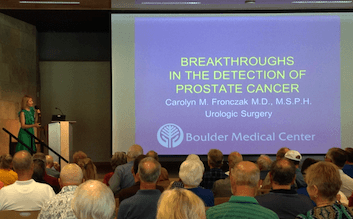
Dr. Carolyn Fronczak, urologist, spoke to an audience of around 100 people about prostate cancer screening
Prostate cancer is the most common cancer in men. In fact, 1 out of 7 men living in the U.S. today will eventually develop prostate cancer. And about 1 in 36 will die from the disease.
“Despite its high incidence, if found early, prostate cancer is one of the most survivable forms of cancer, but early detection is key,” urologist Carolyn Fronczak, MD, told a crowd of nearly 100 people at a recent Boulder Community Health event.
Informed Decision-Making is Key
While prostate cancer screening may detect prostate early, leading medical organizations disagree about who should — and who shouldn’t — get screened.
“Sometimes screening misses the cancer, and sometimes it finds cancer that turns out to be non-aggressive,” Dr. Fronczak explained.
That’s why the American Cancer Society recommends informed decision-making when it comes to having a test to check for prostate cancer.
“Men shouldn’t rush into routine prostate cancer screening, but instead have full, thoughtful conversations with their doctors about the uncertainties, risks, and potential benefits of screening. Together, you and your doctor can decide whether prostate cancer screening is right for you,” said Dr. Fronczak.
The discussion about screening should begin at:
- Age 50 for Men Who are at Average Risk of prostate cancer
- Age 45 for Men at High Risk of developing prostate cancer. This includes African American men and those who have a first-degree relative (father, brother, or son) diagnosed with prostate cancer at an early age (younger than age 65).
- Age 40 for Men at Even Higher Risk (those with more than one first-degree relative who had prostate cancer at an early age).
Basic Screenings for Prostate Cancer
There are two main initial screening tests for prostate cancer:
- Prostate-specific antigen (PSA) test. This is a blood test to check the level of prostate-specific antigen in your blood. Most healthy men have PSA levels under 4 nanograms per milliliter of blood. However, PSA has a limited sensitivity for prostate cancer detection. A lower PSA level doesn’t guarantee a man is free of prostate cancer, and a higher level doesn’t mean he has prostate cancer.
- Digital rectal exam (DRE). During a DRE, a physician inserts a gloved, lubricated finger into your rectum to examine your prostate, which is next to the rectum. Your doctor will feel for size of the prostate and for any bumps or hard areas on the prostate that may need to be tested for cancer.
According to Dr. Fronczak, “A DRE should be done in all men with an abnormal PSA, and a standard initial evaluation combines PSA testing with a DRE.
Additional Prostate Screening Tools
If the results of the PSA and DRE suggest that you might have prostate cancer, your doctor might feel you need a prostate biopsy, which involves using a needle guided by a rectal ultrasound to remove samples of prostate tissue. The tissue samples are sent to a lab, where a specialist will determine the presence of cancer cells.
“Unfortunately, a standard biopsy has risks of pain, infection and may miss the lesion,” Dr. Fronczak warned. “Because of this, the new school of thought is to first recommend a prostate MRI (magnetic resonance imaging) to help identify whether a suspicious lesion may be a cancer or noncancerous tissue.”
Dr. Fronczak and the Boulder Community Health radiology team work together to provide a targeted MRI-guided biopsy of suspected prostate tumors using two types of procedures:
- Multiparametric (mp) MRI: An mpMRI helps not only determine who needs a prostate biopsy but also assists urologists in performing targeted and precise biopsies. “We also use the mpMRI to follow men with elevated PSAs but who have had a negative prior prostate biopsy—just to make sure we didn’t miss a lesion,” Dr. Fronczak said.
- MRI/TRUS Fusion Biopsy: While still new technology, MRI-TRUS fusion technology is being used more often for prostate cancer biopsy and diagnosis. This technology blends (fuses) images from an MRI scan and live transrectal ultrasound (TRUS) for a more detailed view of the prostate. “This is the latest testing improvement for detecting prostate cancer. It can show hard-to-find lesions and increases finding high-risk tumors by 18 percent,” said Dr. Fronczak.
Urologists are also examining biomarkers — molecules secreted by a tumor — in blood and prostate tissue to better diagnose prostate cancer. The presence of certain biomarkers can indicate both normal and abnormal processes in the body. Analyzing these molecular clues helps distinguish between insignificant and significant prostate cancer and identify particularly aggressive prostate cancer. The widely-used prostate-specific antigen (PSA) test is one example of a biomarker screen, however, there are many more that urologists can use for a better understanding of cancer presence and risk.
“Biomarkers give us a probability of finding cancer before proceeding with biopsy and decrease unnecessary biopsies. Still, biomarkers will not detect all cancers,” said Dr. Fronczak. “At this time, no one biomarker can be recommended over another due to lack of head-to-head clinical trials.”
Treating Prostate Cancer
If prostate cancer is found, treatment options depend on several factors, including how fast the cancer is growing, how much it has spread, the patient’s overall health, and the potential benefits or side effects of the treatment.
Treatment can include active surveillance, radiation therapy, chemotherapy, hormone therapy and surgery, such as robot-assisted surgery.
About Dr. Carolyn Fronczak

A Boulder native, Dr. Fronczak attended Sacred Heart of Jesus and Fairview High School. She graduated from Wellesley College, cum laude, with a Bachelor of Science degree in biological science and economics. She earned a Master’s in Public Health and her medical doctorate from the University of Colorado and completed her general surgery and urologic surgery residency at the University of Nebraska.
Dr. Fronczak provides high quality urologic care for both men and women. She specializes in a full spectrum of preventive, non-invasive, minimally-invasive and full surgical treatment options.
Details:
- To Reach the Urology Department, call (303) 440-3093


