
Your allergist can help you navigate confusing symptoms during this time. (photo: Dr. Katie McCormack and a telemedicine visit.)
Coronavirus disease 2019 (COVID-19) is a global viral pandemic that is still affecting our communities. This post aims to help you identify Covid-19, asthma, and allergy symptoms so you can effectively communicate with your doctor and reduce unnecessary urgent care or emergency room visit.
For those with asthma, monitoring your daily health and keeping conditions under control are key components to staying safe during this time. If you develop symptoms such as coughing and shortness of breath, it may be confusing to know if you have asthma, allergies, or a potential virus.
While we do not yet know the impact of coronavirus on asthmatic patients, avoiding infection and regular communication with your doctor is highly important. Your doctor can help you navigate any concerns you may have. We encourage you to first reach out to your regular doctor before proceeding to the Emergency Department or an Urgent care center for any non-urgent concerns. The sooner you reach out to your doctor, the sooner they can help you identify any problems before they become severe and keep you away from facilities where there is a potentially elevated risk of contracting COVID-19.
Be Proactive About Lung Health
 As I mentioned earlier, If you have asthma, you may be at a higher risk of developing complications from COVID-19 and other respiratory viruses. Especially now, you must be proactive about your lung health.
As I mentioned earlier, If you have asthma, you may be at a higher risk of developing complications from COVID-19 and other respiratory viruses. Especially now, you must be proactive about your lung health.
If you have prescribed medications, please ensure that you have at least 30 days supply in your home. Take your medications exactly as they have been prescribed, and don’t hesitate to reach out to your doctor if you have questions.
Do You Have an Asthma Action Plan?
An asthma action plan helps patients maintain control of their asthma, minimizing the risk of asthma attacks, which require urgent medical attention. If you have an asthma action plan, you should follow it. If you do not have one, ask your doctor to give you one. A typical plan is broken down into three color-coded “zones”:
- Green Zone – Breathing is Good
- No coughing or wheezing
- Sleeping through the night without symptoms
- You can work, play and exercise without symptoms
- If you are feeling well, you should continue your usual prescribed daily medications
- Yellow Zone – Use Caution
- First signs of a cold
- Exposure to known asthma triggers
- Cough, mild wheeze, tight chest, coughing at night
- If you are experiencing these symptoms, you may be instructed to increase your home medications or use your emergency inhaler more frequently. If you are unsure, ask your doctor
- Red Zone – Danger
- Your asthma is getting worse fast, and medication is not helping
- Your breathing is hard and fast
- You are having trouble speaking
- In children, their ribs may show when breathing
- If you are in the red zone, contact your doctor immediately
- Do not wait. If you cannot reach your doctor’s office, go to the nearest emergency department
COVID-19, Emotions, and Seasonal Allergies
Strong emotions are known to trigger asthma attacks. If you feel overwhelmed, stressed, or anxious about the COVID-19 virus, please speak to your healthcare provider about additional resources that may help you manage.
Asthma is also commonly triggered by allergies. Seasonal allergies may have similar symptoms to viral illnesses such as a runny nose, sneezing, and congestion. While there is some overlap in infection and non-infection symptoms, infections often cause fever, while allergies do not. The CDC lists the three most common symptoms of COVID-19 as fever, cough, and shortness of breath.
If you have pollen allergies that start in spring, you should begin treatment NOW. Don’t wait to start treatment when the pollen counts rise, and your symptoms worsen. Starting treatment now will not only help you feel better through the entire allergy season by getting a head start, but it may also minimize typical allergy symptoms that could be confused with a viral infection such as COVID-19.
If you are not sure if you have seasonal allergies or do not know how to treat them, speak to your doctor, or schedule an evaluation with an allergist.
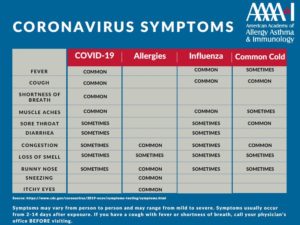 See the full symptom chart that compares COVID-19, influenza, and colds.
See the full symptom chart that compares COVID-19, influenza, and colds.
 Video Visits Now Available…
Video Visits Now Available…
Katherine McCormack, MD – Allergist
Dr. Katie McCormack is an Allergy, Asthma, and Immunology Specialist at Boulder Medical Center. She treats infants, youth, and adults for everything from seasonal and food allergies to asthma and eczema.
Dr. McCormack welcomes new patients in her Louisville, Colo. clinic. She regularly sees patients from throughout Boulder County and nearby communities, including Broomfield, Westminster, Arvada, and Golden.
Learn More
- Dr. McCormack’s Full Profile
- Please Call for an Appointment: (303) 440-3083

